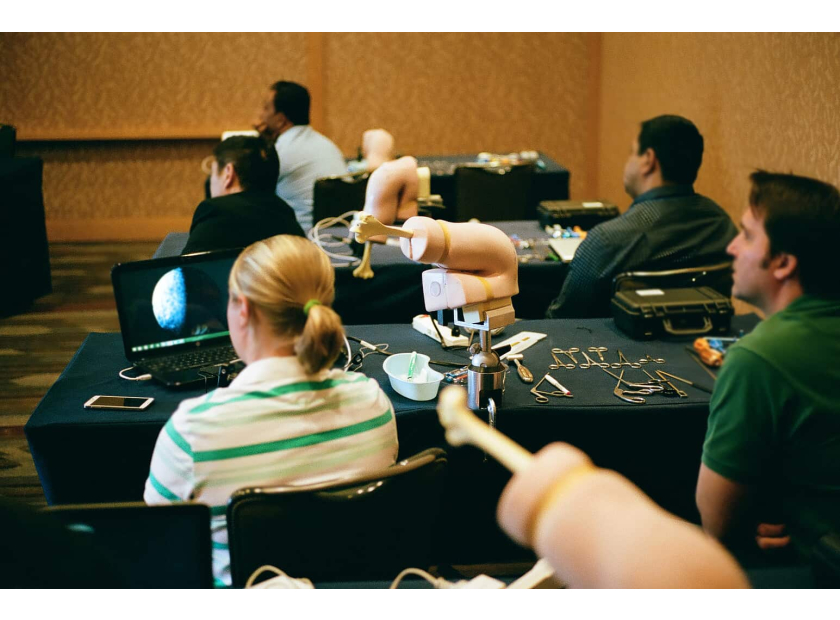
Use Anatomical Models for Hands-On Medical Training
Despite advances in virtual and artificial reality (VR/AR) simulation, physical anatomical models remain an important part of residents’ medical training. Anatomical models facilitate hands-on learning to help residents quickly progress from theory to practice. Let’s take a closer look.
Medical Training Methods
Residency programs have several teaching methods at hand to build up trainees’ anatomical knowledge and procedural skills. These include cadaveric dissection, virtual and artificial reality simulations, and anatomical models used in learning sessions. Of the three, an argument can be made for anatomical models as regularly providing the best hands-on learning experience for residents.
For one, cadaveric specimens are not well-suited to repeated hands-on training, as specimens are generally difficult to obtain for regular teaching sessions, and there are also health risk concerns. While some institutions try to work around this issue by using prosections—a method wherein a demonstrator dissects a specimen in view of a group of students—this approach further lessens hands-on training and experience. Lastly, cadaveric specimens pose an emotional barrier to learning that can slow individual progress from theory to practice.
VR/AR simulations, on the other hand, are progressing rapidly in medical training but still face several challenges. Cost is a major barrier for most institutions in light of reduced funding and fluctuating student populations. Sophisticated systems also require user training for both instructors and participants. It is also known that VR/AR causes side effects including nausea, eye fatigue, and dizziness.
Another issue is accessibility, as VR/AR systems are limited to a certain place and schedule. Lastly, VR and AR's effectiveness in advancing residents from theory to practice through artificial environments is open to debate.
Anatomical models offer a middle ground to both of these methods. Though they can be perceived as a static medium for learning, physical models facilitate repetitive hands-on training better than cadaver dissection and artificial simulation. Here’s why.
Advantages of Anatomical Models in Medical Training
Anatomical models offer many benefits to residents in training. Here are three major advantages:
Low-Cost Material
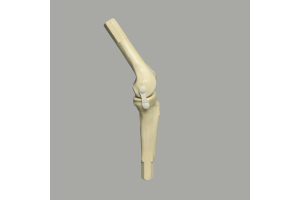
Compared to cadaveric specimens and simulations, physical models are more easily procured at a lower cost. A variety of high-quality models have also been developed for residents to practice surgical procedures such as cutting, reduction, and fixation, among others. Even so, high-quality and full-detailed anatomical models still cost less compared to procuring a temporary specimen or setting up a simulation system that may become outdated as new innovations enter the market.
Hands-On Training
Physical models effectively facilitate repetitive hands-on training among residents. Repetitive practice is key to building procedural confidence and competence. Moreover, anatomical models:
- Pose no emotional barriers or health risks to users.
- Enable mock examination and procedures.
- Are designed for repeated and long-term use.
- Are always available and easily accessible.
- Are tactile and kinesthetic in nature.
- Require no technological setup or special handling.
- Offer students greater freedom in manipulation and interaction.
Models recreate the experience of interacting with physical bones and muscles in a conducive setting without the constraints of time, cost, or accessibility. As a result, residents can progress from theory to practice more quickly in medical training.
Student-Directed Learning
Finally, and perhaps most importantly, anatomical models enable self-directed learning in residency programs.
Anatomical models give medical students a starting point for visualizing several scenarios. A simple, physical model provides residents with a clean slate for creativity. This is harder to achieve when learning is facilitated in a digital environment with templated content. Furthermore, increased information input from simulation competes for mental energy and diverts the brain into processing data instead of engaging in critical thinking.
In the same way, anatomical models allow residents to focus on practicing key technical skills instead of dealing with emotional barriers present when handling a cadaveric specimen.
Using anatomical models, residents and medical students can dictate the pace and extent of hands-on practice according to their own learning styles.
In summary, anatomical models offer greater benefits to residents in medical training compared to the use of cadaveric specimens and simulation systems. Models are easier to obtain and cost less, even for specialized uses such as training for surgical and arthroscopic procedures. Physical models best recreate the hands-on experience of interacting with bones and muscles in a setting conducive to learning. Lastly, anatomical models provide residents and medical students with a clean slate for engaging in critical thinking in medical training.
Best-in-Class Anatomical Models For Medical Training
Sawbones' expertise is built on 40 years of manufacturing and designing the best medical training products for residents, instructors, students, sales specialists, and more. We offer a wide variety of products including:
- Training Models
- Display Models
- Orthopaedic Models
- Patient Education Models
- Biomechanical Models
- Veterinary Models
- Digital Anatomy Media
- Workshop Rentals
We also offer customized products including models and custom displays for all medical training and residency program needs. Sawbones is a proud partner of several medical training institutions, including the Postural Restoration Institute® and Medical Sales College.