Medical Education Models: Effectiveness in Training Exceeds Initial Costs
When it comes to preparing young medical professionals, modern medical education training models’ effectiveness has reached standards that now rival prevailing methods. Engineered solutions with advanced features such as haptic response are currently cheaper than digital, cadaveric, and animal models, and research suggests they’re just as effective in transferring procedural skills to the operating room.
Given the high cost, limited availability, and perceived threat to patient safety involved in the traditional “see one, do one, teach one” approach that has dominated medical education for a century, the current generation of elite models could provide a lasting benefit that far exceeds the price of outfitting an institution with the latest offerings across a range of specialties.
Research and anecdotal evidence already suggest that medical educational models can produce:
- More engaging medical lessons
- Reduced learning times for surgical procedures
- A shift from time-based to competency-based training
- Significant savings through repeat use
- Transferable skills that reduce duration, complications, and errors in practice
The initial cost of the latest generation of medical models buys learning tools that are robust enough for repetition and reuse, authentic enough to build student engagement and confidence, and, most importantly, effective enough to phase out an expensive reliance on operating-room education.
The Next Generation of Medical Education Models
The current generation of medical training models is more dynamic, authentic, and effective than anything previously available. In fact, it might be argued the longevity of Dr. William Halsted’s famous axiom endorsing operating room learning, mentioned above, may be due to the late arrival of viable non-biological alternatives.
At any rate, today’s offerings have a range of advanced features that appeal to teaching institutions, including:
- Haptic feedback. Provides a dynamic, real-time response to student movements and decisions.
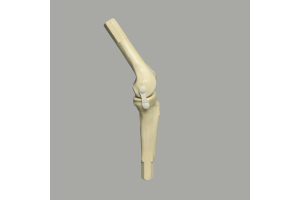
- Composite bone and tactile materials. The authentic feel and performance of modern models prepare students for the physical realities of surgery.
- Dual usage and buildable models. These allow students to train on arthroscopic and open settings and can be expanded to stimulate progress.
- Rigid, reusable materials. Strong enough to withstand use across cohorts.
- Interactive simulations. Models can be used to simulate complex procedures from joint replacements to keyhole surgeries.
The impact of these features is only realized in the context of a medical education model’s effectiveness in producing confident students with skills that are readily transferable to the operating room.
These models start providing education ROI right from the earliest classroom settings.
1. More Engaging Medical Lessons
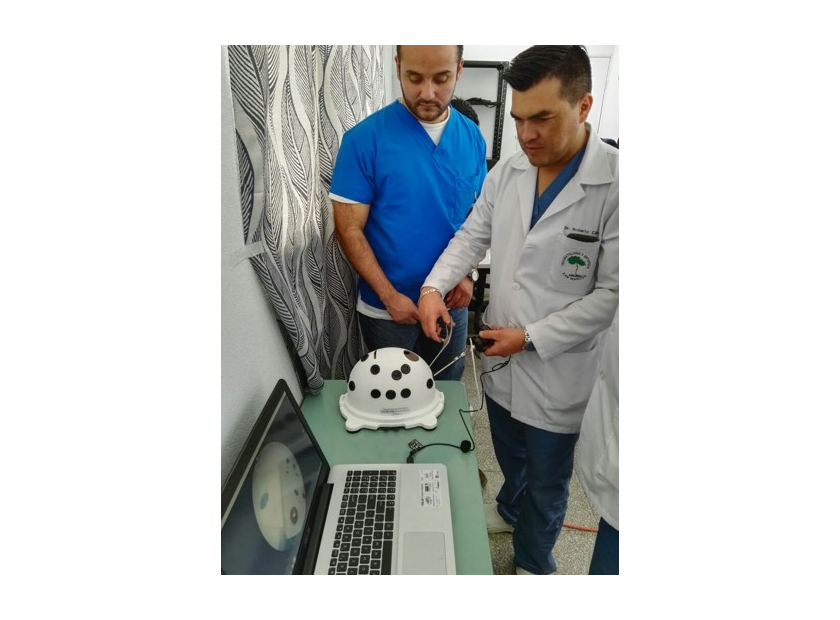
Research has found that student engagement in lessons is strongly related to teaching effectiveness. The use of models and tactile teaching methods has produced better responses in medical students than the traditional one-sided flow of information in a standard lecture.
The dynamic and authentic nature of the current generation of medical training models makes them an obvious vehicle for introducing the base concepts that will form a surgical career.
2. Reduced Learning Times for Surgical Procedures
Mastery of medical procedures requires repetition—lots of it. The realities of operating room availability, however, can make it problematic to give every student in a cohort the necessary exposure to live conditions. Fortunately, recent research suggests that the use of simulation technologies reduces the learning times needed to master surgical interventions early in a specialist’s career.
Repeated exposure to authentic models that can be adjusted to simulate a variety of presentations, settings, and open and closed procedures can build a doctor’s confidence as well as the biomotor skills needed to practically navigate the latest technology and tools.
3. A Shift from Time-Based to Competency-Based Training
Breaking the reliance on operating room exposure in medical training means the parameters of education can be reassessed. Instead of a trial-and-error approach based on supervision, at potential risk to a patient, the use of even low-tech bench models can result in a shift toward competency-based assessment. A student isn’t judged on their expensive exposure to the operating room, but rather on their proven ability to perform a task in simulation on a model. In much the same way that pilots learn and then upgrade their talents in the risk-free environment of a simulator, students and even experienced medical minds can be taught highly specialized techniques in a limited amount of time.
4. Significant Savings Through Repeat Use
One of the chief reasons that engineered medical models are cheaper to purchase and use than cadavers, animal models, or virtual and augmented reality offerings is that they are more robust and more practical. Digital alternatives require advanced equipment and maintenance, while biological models are difficult to attain, offer limited use, and expensive to clean up.
Engineered solutions, on the other hand, are robust enough to withstand the examination of several cohorts, easily stored and reused, and can be modified for future use. Furthermore, the medical education model's effectiveness means their use by many students amplifies the cost benefit relationship—they provide more bang for the buck.
For example, in a recent report published in Nature, researchers found that ocular surgery simulation models that could be reused by students had led to direct financial savings and reduced surgical complication rates among junior doctors.
5. Transferable Skills that Reduce Duration, Complications, and Errors in Practice
Finally, there is a growing amount of research that shows the use of medical models enhances the performance of young physicians across several indicators of a successful operating room outcome. These include:
- A reduction in procedure duration
- A reduction in procedural complications and errors
- Improved clinical communication
- Improved student confidence
The development of transferable surgical skills is the true measure of a medical education model’s effectiveness, but the fact that such a transition can be achieved within standardized teaching environments means the production of competent specialists can become reliable and routine.
In other words, the cost of a single model can be repaid many times over.
A Medical Education Model’s Effectiveness Is Revealed in Practice
The real ROI a teaching institution receives from a state-of-the-art medical training model is the growth in reputation that highly skilled graduates generate. These models are proven to encourage student engagement and confidence, to reduce the learning surgical learning curve, and to provide practical operating room benefits that lead to successful patient outcomes.
Investing in the most advanced models currently being produced places an institution in a better position to succeed.
Sawbones produces a wide range of medical education models to support training across a range of specialties. Visit our contact us page or call us at 206-463-5551 to learn more.

If you're seeking something you can't find on our website, our sales team is happy to help. We can either direct you to the right model or provide a free quote on the right custom project to meet your needs. Discover options with our clear bone models, laminated blocks, custom displays, or other machining projects.